For the record, I’m all for...
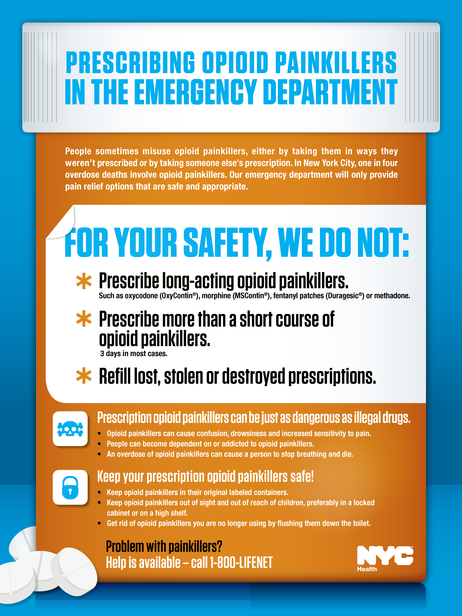
Emergency
Hint: Roche stinks, and the Cochrane...
Okay, it’s not hilarious, it’s funny...
Why we should be very wary...
The Defikopter is a UAV that...
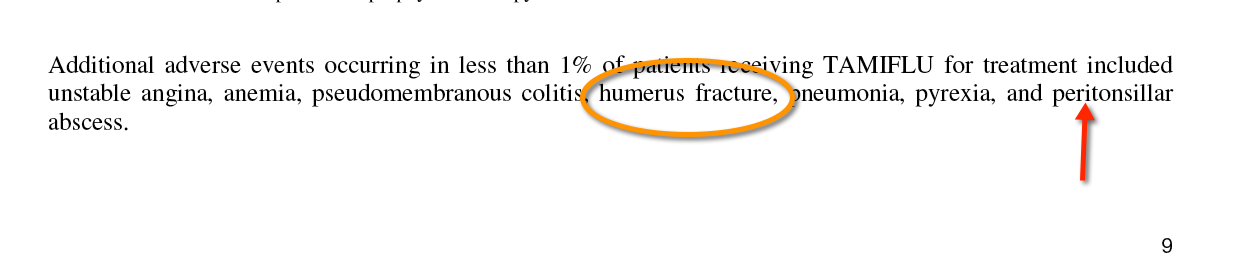
There’s a weird risk factor. What’s...
At the Fort Worth Municipal building,...
We all die. Here’s just a...
Dear Sirs, First, thank you for...
More TPa for stroke… Delusions of...
From NPR: Doctors who follow the...
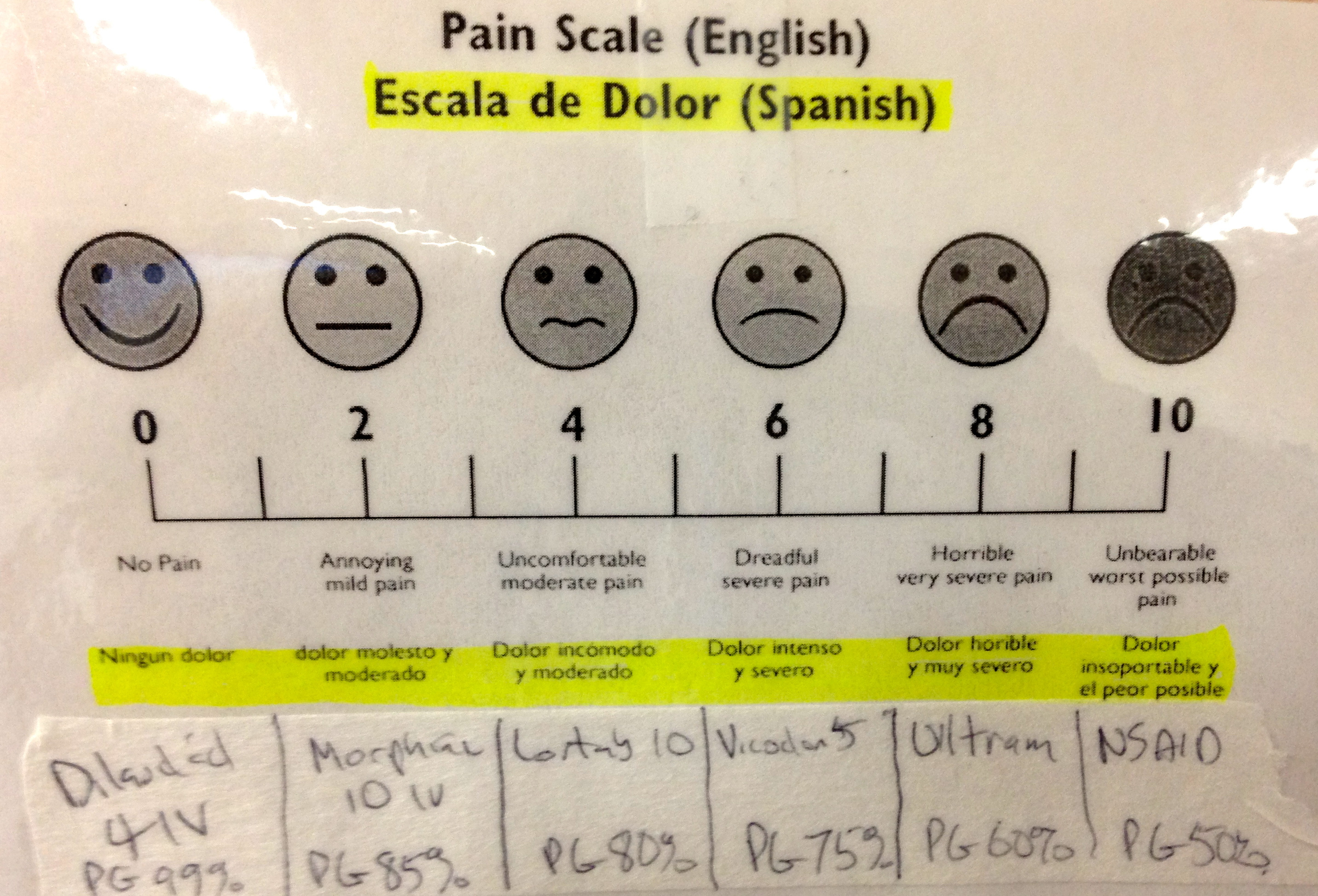
For those not actively engaged in...
Those who don’t follow me on...
Wow. Amazing. AURORA, Colo. — More...
[blackbirdpie url=”https://twitter.com/gruntdoc/status/234183229823922177″]<!-- AddThis Advanced Settings above...