Recently, I blogged about being at...
Emergency
[blackbirdpie id=”223480429871767552″] This reminds me of...
This is my renewal year for...
Stick with it. I’m good at...
Wow. Short, and sweet, and painful....
Let’s say, hypothetically, you could design...
The irony here is that Eli...
If you don’t follow me on...
It’s in San Francisco this year,...
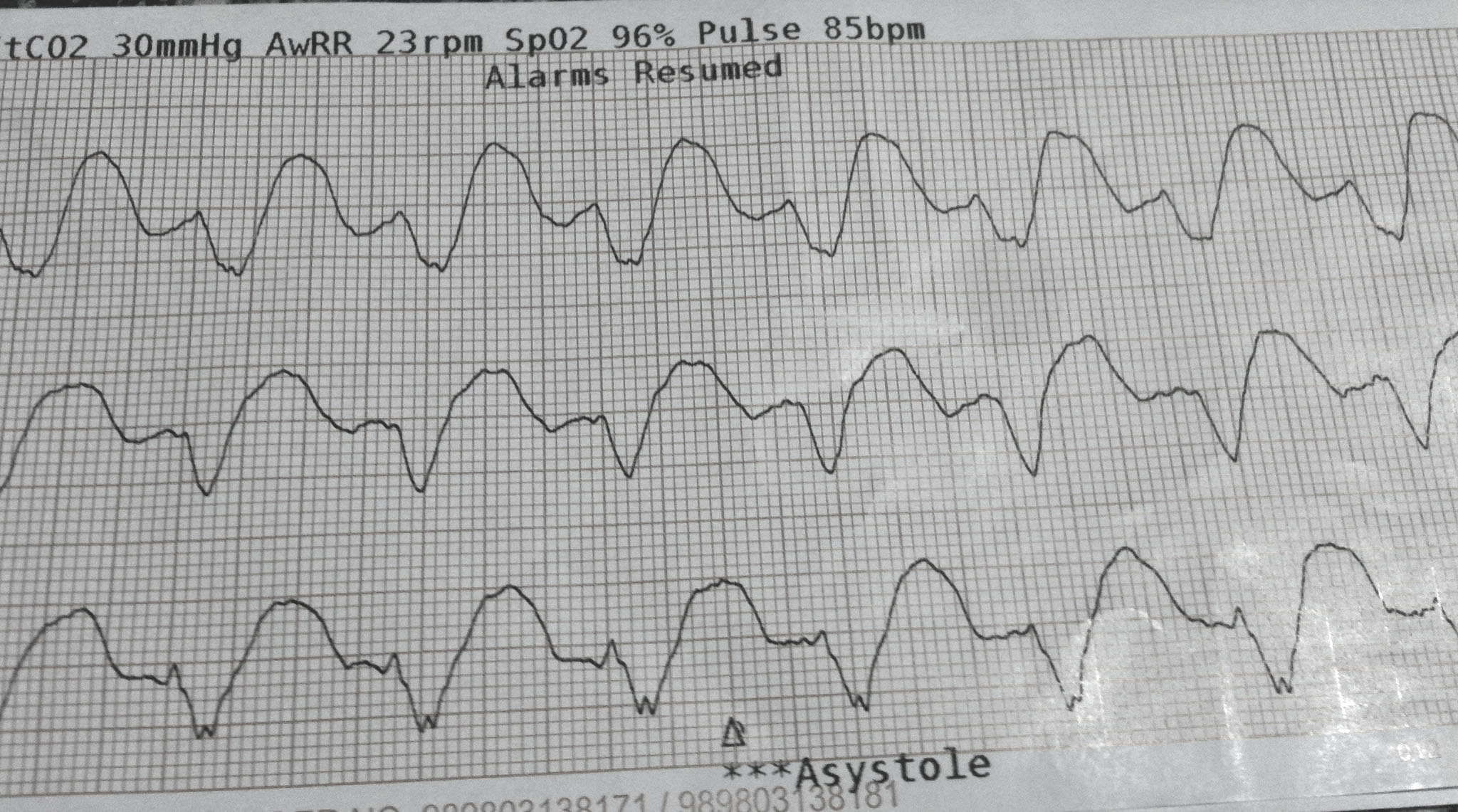
Via hqdmeded.com: 20 yo M with...
Gastroenterologist Michael Kirsch put up a...
“Would any EMS unit that can...
Kudos to MedStar (our Fort Worth...
I walked into one of my...
Okay, it’s kind of amusing, and...