Well that got awkward quickly. “@CardioNP:...
Medical
Apparently they’re blocked, not visible on...
EVD: ebola virus disease; kills 70%...
@nbcdfw What’s that plane’s N-number?<!-- AddThis...
RT @Apathetic_Cynic: Who’s getting married? “@gruntdoc:...
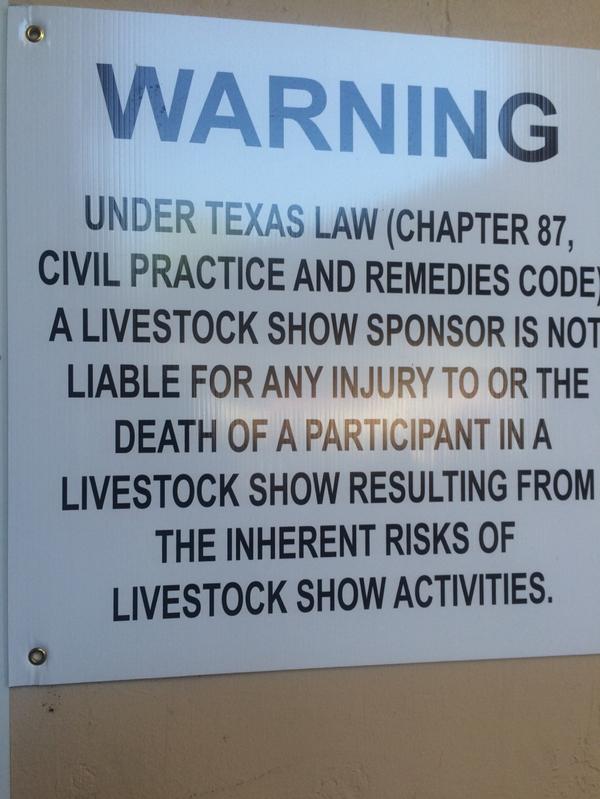
FYI. pic.twitter.com/o7Y0ZFVbpY<!-- AddThis Advanced Settings above...
RT @HarrisonReedPA: If I told you...
@monashanaes @ketaminh @MDAware hardest hit<!-- AddThis...
RT @jimgeraghty: “I’m sorry, sir, your...
Oops. Thanks for the heads up....
RT @jeffbware: @gruntdoc @Skepticscalpel as per...
@doconskis @mdaware @cbsdfw @aceofspadeshq Defining illness...
.@cbsdfw @aceofspadeshq Outside immunosuppression, 99.5 is...