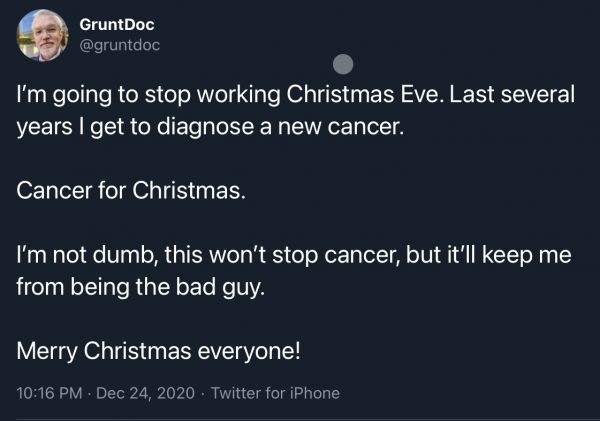
I’m starting this post with a disclaimer, and while it’s been a hell of a lot of days since I posted, disclaimers are only an occasional thing. Generally. So my return starts with a disclaimer.
Please enjoy this setup Tweet, and enjoy the foreshadowing:
Let’s start with the premise, and then I’ll fill in the details. Who is the best person to break bad news? Short version, it’s an ER doctor! Why??? Well, let’s get into that.
When in med school one of the thousands of papers we were assigned (I think it was my preventive medicine class but I cannot swear), one was about how to break bad news, and it was full of the excellent info about the ‘how to’ and I’m not going to address that, there are a zillion pages on giving bad news. What it did go into later and kind of an afterthought was the WHO should break bad news, and as a med student interested in EM (*wavered, long story) the recommendations and the why stuck with me.
(I’d love you tell you what paper it was, and I’ve done (internet searches) and cannot find it, but, here’s what I remember, and all errors are mine should I get this wrong):
First, a survey was done of patients with horrible (cancer) diagnoses, and the patients’ relationship with the person who told them their diagnosis, and
Second: ?did that potential relationship damage affect their ongoing treatment relationship.? You’ll never guess, but yes! If someone the patient knew and trusted told them a terrible diagnosis the patient did hold that against the doc who told them the bad news. This might easily affect the patients’ adherence to treatment (not to mention the psychological resistance to treatment). So, let’s think this through, and again this is from my remembrance of a paper written a while ago.
What the authors (IIRC) thought were important for breaking bad news:
1: The person giving bad news should be involved in the patient’s care,
2: The person giving the bad news should be a credible source,
3: If the person doing 1&2 were doctors involved in the patents’ long term treatment, resentment was very common in the patients and often it interfered with treatment compliance,
BUT,
4: If the doctor giving the bad news was NOT involved in the patients’ longitudinal treatment several things happened: a) While the doctor giving the bad news was in retrospect not liked (and could be disliked), they were respected as they were involved in the patients’ immediate treatment, so they were believed, and b) as they weren’t involved in the patients’ future treatment their absence meant there wasn’t a trust issue with the ongoing treatment team.
I remember being a MS1 (maybe 2, it was all a blur) and thinking: FINALLY, someone has an actual recommendation for how to talk to patients, and it speaks to me.
And ‘tis is my burden and my role to this day:
I’m an ER doc, and it’s MY JOB to be the bad guy for those with a long term bad/tough diagnosis.
You/your relative has cancer, and we will refer you to the right people, I will make sure you have pain medicines to the best of my ability, etc. Patients and their families yell at me, call me names, and I absorb it to be diffused away on the drive home if I’m lucky or a day or three if not, I’m not real to them, it’s grief being released. Shock and pain need an outlet, and damn if being their target isn’t my role, too.
Compassion matters and delivery matters but there’s only a few ways to say the words cancer and prognosis and it doesn’t matter the words past cancer… because nothing is heard for a long time. So I stop. I wait. The questions come, the pleading starts, and were I a deity I’d grant their desires and wishes but I’m just a guy, with a lot of training and experience which translates directly to shit to them as now it’s ‘what do we do and what medications’ and it’s a lot to absorb while realizing none of my responses are answers, I have nothing to offer but plans and hopefully non-awful platitudes (“Diagnosis drives treatment and prognosis, don’t sell the farm , lets see what the actual diagnosis is’)( and by the time I leave the room they all hate me)*.
*They don’t hate me. They hate the situation/diagnosis/sudden change in their condition, the reality of mortality, the reality that control over our lives is an illusion and I’m the one who jarred their reality. For that I get their opprobrium, and I know that’s my role. Hopefully this means their oncologist, their surgeon/oncologist/whatever they need to get better can displace their anger/blame energy to me, so their treatment team is innocent of the change in their life from before to after diagnosis.
An aside, when I was diagnosed with prostate cancer (very long story) I already knew all of the above, and didn’t think a thing about the messenger. Sure, I have a lot of advantages, but one is knowing the person who gives the bad news isn’t the enemy.
To sum up:
patients need diagnoses, especially if it’s not good
ER docs are the right docs to do this
That makes it awful and hard, and love and protect your kids, and your companions.