Geez, the NY Times (obscure liberal paper in the Northeast) has interviewed several neurologists (and exactly one Emergency Medicine Physician) and has written a four-page article on stroke. They got little right.
It’s a tour-de-force in obfuscation of fact, presentation of tragedy as preventable, and the presentation of TPA as an ignored wonder-drug, MRI should be the standard of care for new strokes, and frankly there’s no redeeming value within. Nevertheless, I shall persevere, and even if it makes nobody other than me happy, I shall fisk to my hearts’ content. (Many thanks to Notes from Dr. RW for bringing this to my attention, and for taking the hit for the rest of us and reading the NY Times, you poor wretch).
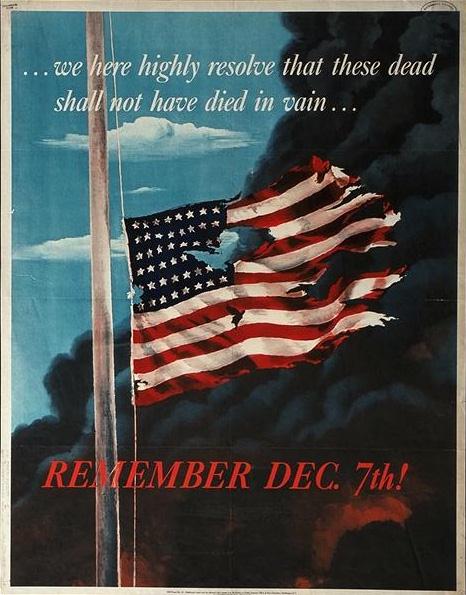
I was going to address this in the article as I got to it, but it’s too good / on point to bury below the fold. Here’s all you need to know about tPA for CVA (from AAEM), in a nice graphical form:
Lost Chances for Survival, Before and After Stroke
By GINA KOLATA
Dr. Diana Fite, a 53-year-old emergency medicine specialist in Houston, knew her blood pressure readings had been dangerously high for five years. But she convinced herself that those measurements, about 200 over 120, did not reflect her actual blood pressure. Anyway, she was too young to take medication. She would worry about her blood pressure when she got older.
Then, at 9:30 the morning of June 7, Dr. Fite was driving, steering with her right hand, holding her cellphone in her left, when, for a split second, the right side of her body felt weak. “I said: ‘This is silly, it’s my imagination. I’ve been working too hard.’ ”
Suddenly, her car began to swerve.“I realized I had no strength whatsoever in my right hand that was holding the wheel,” Dr. Fite said. “And my right foot was dead. I could not get it off the gas pedal.” …
Dr. Fite is one of an estimated 700,000 Americans who had a stroke last year, but one of the very few who ended up at a hospital with the equipment and expertise to accurately diagnose and treat it.
Dr. Fite has been active in the practice and politics of Emergency Medicine for a good while, and I was unaware of her stroke. I hope she’s recovering well.
Stroke is the third-leading cause of death in this country, behind heart disease and cancer, killing 150,000 Americans a year, leaving many more permanently disabled, and costing the nation $62.7 billion in direct and indirect costs, according to the American Stroke Association.
But from diagnosis to treatment to rehabilitation to preventing it altogether, a stroke is a litany of missed opportunities.
Many patients with stroke symptoms are examined by emergency room doctors who are uncomfortable deciding whether the patient is really having a stroke — a blockage or rupture of a blood vessel in the brain that injures or kills brain cells — or is suffering from another condition. Doctors are therefore reluctant to give the only drug shown to make a real difference, tPA, or tissue plasminogen activator.
This is a truckload of hooey. Any Emergency Physician worth the title does this for a living, and while it’s challenging to sort wheat from chaff, it’s why Emergency Medicine exists as a specialty. Yes, there is a tremendous differential diagnosis, but that goes with the territory. And reluctance to administer tPA for stroke is more than reluctance, there are solid reasons to be very very careful with the decision.
Many hospitals say they cannot afford to have neurologists on call to diagnose strokes, and cannot afford to have M.R.I. scanners, the most accurate way to diagnose strokes, for the emergency room.
Call schedules are dependent on the number of neurologists eligible for call, and MRI scanners are expensive, but from what I’ve been told they pay for themselves within a year or so. That’s not to say that MRI is the standard of care for an acutely altered mental status (it’s not), but pretty much every actual ED in the US has a CT scanner, and that IS the standard of care. This focus on the MRI throughout the article is mission creep for stroke that’s not currently justified.
Although tPA was shown in 1996 to save lives and prevent brain damage, and although the drug could help half of all stroke patients, only 3 percent to 4 percent receive it. Most patients, denying or failing to appreciate their symptoms, wait too long to seek help — tPA must be given within three hours. And even when patients call 911 promptly, most hospitals, often uncertain about stroke diagnoses, do not provide the drug.
No, it’s not ‘uncertainty of the symptoms’ it’s reality that there are a lot of exclusion criteria for tPA for CVA, and given the stakes if it’s gotten wrong it’s very serious.
“I label this a national tragedy or a national embarrassment,” said Dr. Mark J. Alberts, a neurology professor at the Feinberg School of Medicine at Northwestern University. “I know of no disease that is as common or as serious as stroke and where you basically have one therapy and it’s only used in 3 to 4 percent of patients. That’s like saying you only treat 3 to 4 percent of patients with bacterial pneumonia with antibiotics.”
If antibiotics directly killed 3-4% (his number) of pneumonia patients, there would be a reticence to use them, too. This is a straw man, and isn’t worth more discussion.
And the strokes in the statistics are only the beginning. For every stroke that doctors know about, there are 5 to 10 tiny, silent strokes, said Dr. Vladimir Hachinski, the editor of the journal Stroke and a neurologist at the London Health Sciences Centre in Ontario.
“They are only silent because we don’t ask questions,” Dr. Hachinski said. “They do not involve memory, but they involve judgment, planning ahead, shifting your attention from one thing to another. And they also may involve late-life depression.”
These typically don’t present to the ED, and when they do there’s an utterly enormous differential diagnosis to go through before ‘stroke’ is considered. Even if ‘stroke’ is the diagnosis for these patients’ presentations, their NIH Stroke Scale would be 0 or 1, and they would never be candidates for TPA in the first place.
…
One Tuesday morning in March, Dr. Steven Warach, chief of the stroke program at the National Institute of Neurological Disorders and Stroke, met with a team from Washington Hospital Center, the largest private hospital in Washington, to review M.R.I. scans of recently admitted patients. They were joined in a teleconference by neurologists at Suburban Hospital in Bethesda, Md., the only other stroke center in the Washington and suburban Maryland area. …
The images were mementos of suffering.
Their suffering is not to be minimized, it’s real. And, there’s no information given to tell which would or would not have arrived in the ED in the time to even be considered for tPA. This is an attempt to conflate bad outcomes with uncaring, or negligence, which is hooey at best and journalistic malfeasance at its worst….
But what was perhaps saddest to the neurologists viewing the M.R.I. scans that morning was that tPA, which only recently appeared to be a triumph of medicine, had made not a whit of difference to these patients. They either had not arrived at the hospital in time or had been considered otherwise medically unsuitable to receive it.
Aah, there you go. Excluded by time to presentation. This revelation waits until the heart-strings have been fully tugged, mind you.
Few would have predicted that fate for the drug. In 1995, after 40 years of trying to find something to break up blood clots in the brain, the cause of most strokes, researchers announced that tPA worked. A large federal study showed that, without it, about one patient in five escaped serious injury. With it, one in three escaped.
A study which has yet to be recreated in actual use. Real-life experience has been much less sanguine in its risk-benefit ratio.
The drug had a serious side effect — it could cause potentially life-threatening bleeding in the brain in about 6 percent of patients. But the clinical trial demonstrated that the drug’s benefits outweighed its risks.
This is where EM docs say “huh”? So, even given it “only” causes 6% of patients to have hemorrhages into the brain, those patients die or if they survive they’re worse off than before, and that’s when they were having a stroke! So, a stroke patient (living, with a stroke) is converted to worse or dead. This is one of the big, big bones we have to pick with this therapy.
When the study’s results were announced, Dr. James Grotta of the University of Texas Medical School at Houston expressed the researchers’ elation. “Until today, stroke was an untreatable disease,” Dr. Grotta said.
But the expected sea change did not occur.
One problem was that patients showed up too late. Many had no choice. Strokes often occur in the morning when people are sleeping. They awake with terrifying symptoms, paralyzed on one side or unable to speak.
“That’s the challenge — we have to ask the patient” when the stroke began, said Dr. A. Gregory Sorensen, a co-director of the Athinoula A. Martinos Center for Biomedical Imaging at Massachusetts General Hospital. “If they don’t know or can’t talk, we’re out of luck.”
Simplisme. If we can reasonably infer, it’s not exclusionary for the three hour window.
Another problem is deciding whether a patient is really having a stroke. A person who has trouble forming words could just be confused. Or what about someone whose arm or leg is weak?
“A lot of things can cause weakness,” Dr. Warach said. “A nerve injury can cause weakness; sometimes brain tumors can be suddenly symptomatic. Sometimes people have migraines that can completely mimic a stroke.”
In fact, he said, a quarter of emergency room patients with symptoms suggestive of a stroke are not actually having one.
Hello? Is this thing on? One fourth of patients thought to be having a stroke aren’t. Still gung-ho to give tPA?
Most get CT scans, which are useful mostly to rule out hemorrhagic strokes, the less common type that is caused by bleeding in the brain and should not be treated with tPA. Stroke specialists can usually then decide whether the patient is having a stroke caused by a blocked blood vessel and whether it can be treated with tPA.But most stroke patients are handled by emergency room physicians who often say they are not sure of the diagnosis and therefore hesitate to give tPA.
Again a slur against Emergency Medicine Physicians. Yes, there are patients whose presentations are so complex we aren’t sure of their condition. Should we just kill 3% and worsen the other 3% of them? No. Idiocy and advocacy aren’t terribly far apart for this topic.
Dr. Richard Burgess, a member of Dr. Warach’s stroke team, explained the situation: There is no particular penalty for not giving tPA. Doctors are unlikely to be sued if the patient dies or is left with brain damage that could have been avoided. But there is a penalty for giving tPA to someone who is not having a stroke. If that patient bleeds into the brain, the drug not only caused a tragic outcome but the doctor could also be sued. Few emergency room doctors want to take that chance.
I have a colleague friend, and his Emergency Medicine partner has been sued for giving tPA, and for not giving tPA. Tell me again there aren’t disincentives for tPA use, and disuse?
Treatment Barriers
There is a way to diagnose strokes more accurately — with a diffusion M.R.I., a type of scan that shows water moving in the brain. During a stroke, the flow of water slows to a crawl as dead and dying cells swell. In one recent study, diffusion M.R.I. scans found five times as many strokes as CT scans, with twice the accuracy.
A diffusion M.R.I. “answers the question 95 percent of the time,” Dr. Sorensen said.
It seemed the perfect solution, but it was not.
Most hospitals say they cannot provide such scans to stroke patients. They would need both an M.R.I. technician and an expert to interpret the scans around the clock. They would need an M.R.I. machine near the emergency room. Most hospitals have the huge machines elsewhere, steadily booked far in advance for other patients.
It is simply not practical to demand the scans at every hospital or even every stroke center, said Dr. Edward C. Jauch, an emergency medicine doctor at the University of Cincinnati and a member of the Greater Cincinnati/Northern Kentucky Stroke Team.
“If you made M.R.I. the standard of care before giving tPA, most centers would not be able to comply,” Dr. Jauch said. And if it takes more time to get a scan — as it often does — it might be better to forgo it and give tPA immediately if the patient’s symptoms seem unambiguous.
Finally the only EM physician in the article is heard from, and he’s correct: you want diffusion MRI to be the standard? Fine, but about 1/100 potential tPA candidates will get them.
Doctors do not need an M.R.I. to diagnose and treat stroke, said Dr. Lee H. Schwamm, vice chairman of the department of neurology at Massachusetts General Hospital. But, Dr. Schwamm added, if the question is whether it helps, there is one reply: “By all means.”
It has still not been shown, though, that M.R.I. scans actually improve outcomes. It might depend on the circumstances and the hospital, said Dr. Walter J. Koroshetz, deputy director of the National Institute of Neurological Disorders and Stroke.
But some who use M.R.I. scans, and who have studied them in research, say the system has to change. They say enough is known about the scans to advocate having them at every major medical center that will treat stroke patients.
“All these problems could be solved if there was a will to do it,” Dr. Sorensen said. In his opinion, it comes down to old and outdated assumptions that there is not much to be done for a stroke, to financial considerations and to a medical system that resists change. But the most significant barriers, he said, are financial.
Yes, and logistic. I work in a stroke center (fully certified yet not showing up the the given link the JCAHO’s search engine). I, and no doubt my colleagues, have had two potential stroke candidates at the same time. A CT for CVA takes about a minute; a diffusion MRI takes a lot longer, like 30 minutes. Not much time, you say? Empty MRI’s lose money. Nobody has an ‘extra’ MRI machine waiting for another maybe stroke.
Another approach, stroke specialists say, is to direct all patients with stroke symptoms to designated stroke centers. There, stroke patients would be treated by experienced neurologists and admitted to stroke units for additional care. For the first time, in its newly published guidelines, the American Stroke Association recommended the routing of patients to stroke centers.
I work in a designated stroke center. If you come to our ED you’ll be treated by an Emergency Physician. The Neurologists aren’t coming in to see you and your stroke until the diagnosis has been made, and usually until the treatment is underway. Sorry.
But even with such a system in place, many patients end up at hospitals that are not prepared to treat them, as Dr. Grotta discovered in Houston.
He thought he could change stroke care in Houston with the stroke center idea. The first step went well — the city’s ambulance services agreed to take all patients with stroke symptoms to designated stroke centers.
Then, Dr. David E. Persse, the city’s director of emergency medical services, asked every one of Houston’s 25 hospitals if it wanted to be a stroke center. While seven have said yes, others have declined.
Stroke patients, unlike heart attack patients, are not moneymakers. Because of the way medical care is reimbursed, most hospitals either lose money or do little more than break even with stroke care but can often make several thousand dollars opening the arteries of a heart attack patient. And being a stroke center means finding and paying stroke specialists to be available around the clock.
Soon another problem emerged. As many as a third of the patients refused to let the ambulance take them to a stroke center, demanding to go to their local hospital.
“By law in Texas, we cannot take that man to another hospital against his will,” Dr. Persse said. “We could be charged with assault and battery and kidnapping and unlawful imprisonment.”
Umm, not exactly. There are EMS protocols that allow EMS to bypass nice community hospitals for the Trauma Centers for those patients that need them. The same can be done for stroke patients.
The Joint Commission, which accredits hospitals, recently started certifying stroke centers, requiring that the hospitals be willing to treat stroke patients aggressively. But only 322 of the 4,280 accredited hospitals in the nation qualify, and most patients and doctors have no idea whether a hospital nearby is among them. (The list is available on the site http://www.jointcommission.org/CertificationPrograms/Disease-SpecificCare/DSCOrgs/ under “primary stroke centers.”) Some states, like New York, Massachusetts and Florida, do their own certifying of stroke centers.
Nonetheless, most ambulances do not consider stroke center designations when they transport patients. And, said John Becknell, a spokesman for the National Association of Emergency Medical Technicians, national programs can be difficult because every community has its own rules for which ambulances pick up patients and where they take them.
Dang communities, and their local abilities.
As a result, most stroke patients have no access to the recommended care and even fewer get M.R.I.’s, a situation Dr. Warach said he found appalling.
“How can it ever be in the patient’s best interest to have an inferior diagnosis?” he asked. “It borders on malpractice that given a choice between two noninvasive tests, one of which is clearly superior, the worse test is the one that is preferred.”
This is a doctor trolling to be a plaintiffs’ witness. I’m certain he means well, but he no doubt works in an Ivory Tower with all the resources he thinks he needs, but this is the sort of statement that gets working ER docs, and their consultants, hanged. Maybe he was misquoted. I hope so.
Averting Catastrophe
In those awful moments when she realized she had had a stroke, Dr. Fite, unlike most patients, knew what to do. She told the ambulance crew to take her to Memorial Hermann Hospital, even though it was about an hour away. She knew that it was one of the Houston stroke centers, that Dr. Grotta worked there, and that its doctors had experience diagnosing strokes and giving tPA.
When she arrived, Dr. Grotta asked if she was sure she wanted the drug. Did she want to risk bleeding in the brain? Dr. Fite did not hesitate. The stroke, she said, “was just so devastating that I would rather die of a hemorrhage in the brain than be left completely paralyzed in my right side.”
“In my horrible voice, I said, ‘Yes, I want the tPA,’ ” Dr. Fite said.
Within 10 to 15 minutes, the drug started to dissolve the clot.
“I had weird spasms as nerves started to work again,” Dr. Fite said. “An arm would draw up real quick, a leg would tighten up. It hurt so bad I was crying because of the pain. But it was movement, and I knew something was going on.”
Wow, good for her, and her bravery. TPA is often called a ‘walk or die’ drug, which is an overstatement on both sides of the equation, but I’m not so sure I would ask for it, even given the situation described.
…
As for Dr. Fite, she completely recovered. And she has changed her ways.
She was sobered by the cost of her treatment and brief hospital stay — $96,000, most of which was paid by her insurance company. But she was even more sobered by how close she came to catastrophe.
Now, Dr. Fite takes three blood pressure pills, a drug to prevent blood clots and a cholesterol-lowering drug. She plans to take those drugs every day for the rest of her life.
“I was so stupid,” she said. “Boy, when you go through this, you never want to go through it again.”
“I have been given that precious second chance,” she said. “I was so blessed.”
Again, good for her, she’s a lucky person. But none of this says a) tPA should be given for anywhere near every stroke, b) that anything other than a plain CT read by a Board Certified Radiologist is needed, and c) the ‘MRI for acute stroke’ angle is weird agenda-pushing which is NOT the standard of care.
tPA: potentially good, risky therapy.
Emergency Medicine Physicians: not as dumb as made out.
MRI: not the standard of care, except in the NYT.


Thanks for the explanation, GruntDoc. Did you by any chance email this to the reporter? She usually responds within a day, and you can click on her name to take you to her email link.
Incredible as it may seem, the NYTimes reporters are for the most part, very responsive to readers’ comments, and the stance of the Times is pro-physician.
Shocking, I know! 8^O
Well done, sir, well done indeed.
Good job Gruntdoc. Shout it to the world.
Hm. Dr. Fite would have been ruled out as a tPA candidate in my ER (a JCAHO stroke center) for her blood pressure if it was indeed 220/120. I think you have a chance to get it lowered to less that 180 systolic with a couple doses of metoprolol, but after that, no tPA.
I remember when the ‘designated on-call stroke neurologist’ (there’s a call schedule with an on-call stroke neurologist for each shift 24 hrs/day) demanded that I “run the patient to MRI for a DWI scan!”
We have to do: A 1 1/2 page MRI checklist (if the patient can’t talk, he doesn’t know what metal is or is not in his body and they’ll refuse to do the scan unless there are extensive reliable records or a reliable family member present), send the MRI checklist, kick someone else out of the machine, saline lock all the IVs (if they came by medic, this is an extensive operation requiring a complete change-over of IV tubing), get all of the patient’s clothes off and put him in an MRI-compatible gown, find a telemetry nurse able to be dedicated to this patient in an MRI scanner for 30 minutes (usually a resource nurse who is always busy), get the scan read (which, at night, means it has to be transmitted to a radiologist off-site), etc etc…
The neurologist was highly pissed that I was unable to just “run the patient through the MRI scanner” because he said so.
So, yeah, MRI shouldn’t be the standard of care.
Gruntdoc, great job dissecting the article and the issue.
It amazes me how the lay press oversimplifies such a confusing issue, and raises unreasonable hopes and expectations for patients and their families. Most amazing is how the risk of hemorrhage and death is so blithely glossed over.
The articles always seem to include an anecdote where some one gets tpA and jumps off the table instantly cured. This is not supported by the literature where the gains are actually small functional improvements down the road.
there is one ER doc that quite dumb,dr fite, she could have avoided this by get treated for hypertension
AWESOME critique of a bad article.
I seem to remember that tPA doesn’t help right away with stroke. Its benefit is seen months down the road in rehab, a certain percentage of patients who got it had better recovery. So its not a magic bullet where you wake up and your like “Hey, I’m all better”. (different for AMI)
That being said, I have been disappointed by the ER docs in my hospital. But for different, unrelated reasons.
I’ve given some tPA, and am a believer in its benefits. In our hospital, there initially was a lot of inertia involved in getting going with its use. This isn’t blaming anyone, just I think an expected result when you are talking about a powerful drug yet one with risks (I think better than saying “risky drug” — after all, it’s the same tPA used all too commonly for MIs).
It seems to turn out that the more you use the drug the fewer problems (percentagewise) you see. Part of this comes from less handwringing, but also the ED efficiency of the process.
This having been said, I also think that some of the people most vocal about the “need” to use more tPA are unrealistic about the percentage of patients we can ever expect to see get the drug, for a whole host of reasons. I also think it is being more than a little uncollegial to point fingers suggesting that docs are practicing bad medicine by not giving more tPA. Not exactly what I would call a good mentoring technique.
“The articles always seem to include an anecdote where some one gets tpA and jumps off the table instantly cured.”
I’ve even had several patients who when I just thought about giving tPA they immediately got better. What a wonder drug!
(Like the other anecdotes you mention, I think these miracle cures are otherwise known as TIAs)
For the record, I have given tPA when situations warrant, and have not when they didn’t. And, I’ve sweated the decisions in both directions. I’m not a ‘no tPA ever’ guy, but I am deeply skeptical of any population-based therapy with such a tremendous downside.
I work as a paramedic. So I’m well acquainted with the nuances of stroke patients. On the one hand you have people who don’t hesitate to call for chest pain. Yeah, you get a fair percentage who suffer with it for a few days, then call, but most people are quick.
Stroke patients are a different game entirely. I don’t understand why, but you get people who wake up with a limb they can’t move, a mouth they can’t open correctly, and speech that’s slurred. But don’t bother calling. lemme see if I can walk it off.
That one always puzzled me. The time element is critical for effective therapy. Community recognition is a major impediment for stroke therapy. Then there are the systemic problems. EMS recognition of potential stroke patients. Alerting the receiving facility in a timely manner. That facility actually having the apparatus mobilized. Transport to the closest appropriate facility.
But what gets me is the whole kidnapping and imprisonment issue. It’s often communicated that whole kidnapping thing. Particularly in EMS. Oh, you can’t just take them. That’s kidnapping! They have to go where they want!
We take trauma to a trauma center based on trauma routing criteria. We take STEMI to a facility that meets our (the EMS service) criteria for timely treatment of STEMI care. While we don’t have preferential routing criteria (yet) for stroke patients, when I suspect a stroke, I do my best to encourage that the patient consider a facility other than the community hospital. If this isn’t sufficient, I’ll call the community hospital to give report. A good report can get me what I want: orders to divert to a more distant, but more appropriate facility. No community hospital wants to have a patient come in that exceeds their capabilities, and will just have to be transferred by ambulance again.
This can cause much consternation among colleagues, who see this as the sinful process of recommending one hospital over another. I don’t see it that way. I see it as a way of advocating for better patient care. The patient isn’t always aware of hospital limitations. Suburb Health Systems might have served this patient well in the past, but Ghetto General has the tools and staff to treat them best. It’s also a form of informed consent as I see it. Transport to an appropriate facility is an intervention. The same as any other. And interventions should be explained to the patient so they can make an informed choice.
What I find most puzzling is the premise of the article. It’s not as if people are afraid of treating strokes. I have yet to meet a physician who wanted to watch stroke patients suffer increase morbidity out of some fear of litigation. It’s not as if clinicans are opposed to tPA. If anything, the people in the Neuro CCUs wish it could be utilized more often. But it’s the risk:benefit, and the significant contraindications that prevent its use, not fear or hesitation.
Hello to all – I am not a member of the medical community and found this discussion only by searching “stroke tpa 2007”. I will enter the discussion in laymans terms with no direct knowledge of the merits of TPA other than my own experience. I hope that you will respect my perspective even if you feel it is based on ignorance and luck. My pre-stroke meds were Hydrochlorothyazide, Lipator and Prilosec – all taken as prescribed and all known medical conditions controlled effectively by these. I am active in biking, hiking, Cross-country skiing and snowshoeing and in pretty good shape.
I am 61 years old and had a stroke on June 12 of this year. Things started going downhill as I was going out the door with my wife to ride our bikes. Initial symptoms were dizziness and numbness in the right arm. I wanted to just lay down for a while and my wife wanted me to go to the hospital immediately. She won and drove me to the hospital ER in approximately 10 minutes. By the time I reached the hospital my face was sagging on the right side, my right arm swung at my side and my right leg was not functioning.
Our hospital is a rural facility in a small rural community of about 5000 people. I told the ER personnel that I wanted to be considered for “the clot busting drug” as I entered the facility. Yes, it was because of those ads that some find troublesome. The ER doc went through a series of tests and ordered a CT scan. He then called a larger facility with a neurologist on staff and discussed these results. He carefully explained the downside (I particularly recall a 6% mortality figure due to unexpected bleeding) and the upsides to me. The consulting neurologist felt I was a candidate for TPA. I signed the release and took the TPA.
My mother had a stroke when she was 80 and lived to 96. She spent 16 years in a wheelchair wearing a diaper, unable to talk very effectively and having a changed personality (and not for the better). That entered my thinking.
I started regaining function about 15 minutes after TPA was administered and had regained about 90% of functioning over the next hour. I was transfered by ambulance to a larger hospital where a neurologist was on staff for a couple of days and released. I have now, after two weeks, pretty much recovered.
I rode for approximately one and a half to two hours on my mountain bike each of the past three days and go about my life as before the stoke. I continue to have some minor numbness in my right shoulder and in the right cheek. I receive OT services three times a week to work on the shoulder weakness. I seem to be thinking pretty clearly and have no apparent deficits in this area (or at least no new ones!).
For me I believe that the decision to administer TPA was the right one for me. I believe that it was an informed decision and that I am one lucky fellow. While I believe that I understand the nuances of the discussion that comes before my post, I guess I am the proof of the upside of TPA or maybe not. Maybe I would have recovered anyway. Who knows? My only contribution to this discussion is anecdotal. I can appreciate that there needs to be care taken to give the drug only to those who meet the criteria, but I also hope that the procedure for measuring these criteria can be standardized in such a manner to provide risk/benefit data for the patient or caregiver to make an informed decision. I would hope that this medication will become more widely available so that more medical facilities will have the option available for that portion of the population that can benefit.
Excellent critique. What is troubling about articles like this is that they present medical procedures/treatment as if they should be standard of care. Thus, a layperson has little choice but to internalize the message. The contraindications of tPA are rarely emphasized. As such, the public is not sufficiently educated. Indeed, watching a patient’s symptoms resolve following tPA is quite astonishing. Nonetheless, anyone who has witnessed a patient bleed following lytic will have a healthy respect for the drug.
When tPA was first offered at my main hospital, I was part of the neurology/ER/IM panel that evaluated its usefulness. Unfortunately, we found a 40% mortality rate (that means dead) from the tPA at our hospital, and only 1 of the 10 neurologists at our facility now routinely recommend using it after a normal CT brain.
I remember an evening news show (20/20?) a few years ago interviewing a “stoke” patient and dramatically re-enacting his “stoke” and his instantaneous, miraculous recovery upon being given tPA. “It saved my life!” It did not discuss the incidence of bleeding, TIA (“stroke” completely resolved within 24 hours), RIND’s (resolved within 7 days), or other “strokes” that spontaneously resolved. And it did not mention the risk of bleeding around the edges of a large stroke. Or that most younger population stoke victims resolve most of their symptoms over time. Or that CT scans don’t “diagnose” stroke, but only demonstrate a BLEEDING type of stroke (most of the time).
I’ve taken to showing the AAEM form above to patients and their families when explaining to them why tPA is not a slam-dunk treatment, and have prevented treating a lot of TIA’s with tPA. Drug companies get $4,000 per shot for tPA – sorry, guys, it ain’t for everybody.
But I do agree with Movin’ Again Al – when it works correctly, tPA is an incredible drug. I just hate seeing someone bleeding into their brain and dying from what could have been treated with less dangerous drugs. Even with MI’s (heart attacks), stat use of the Cath Lab is indicated more often than tPA.
Having worked in the stroke center mentioned in the article, with one of the physicians interviewed in the article, I can safely say that a) we use CT head on a stroke protocol when the patient hits the door; MRI is only used if there is question about the diagnosis, or after tPA, or if it’s too late to do tPA but we need to know extent of the damage. b) They’re not afraid to push the plunger for tPA for patients who qualify, but they’re certainly not going to give it to anyone with contraindications (the checklist is a page long). c) Even then, I only saw it used a few times on the rotation because most patients showed up too late or had contraindications.
So even one of the doctors interviewed in the article, who works in a stroke center, isn’t pushing for MRI in acute stroke patients when assessing for tPA.
My mother died last month of a stroke. She had leg pain sometime in the morning not sure it’s related. Took a walk with my father to loosed her leg then around 10:00 am she had a stroke. She went to the hospital and they admininstered TPA. Not sure what time they administered the TPA, I’ll have to ask my father or sister. I live a few hours away. By the time I got to the hospital, she was unconscious. Her brain was bleeding. By 4:00 am they declared her brain dead. I’m starting to wonder if someone messed up. She also had some vision issues a days before but not sure if she mentioned it to the ER. I’d be wary of taking the TPA, it killed my mother.
You are 100% right!
I’ve been through this with both parent in the last 5 years – Dad once with TPA very successfully, and Mom once successfully with TPA. Yesterday Mom had another stroke (hemmorhagic) and because of a lung tumor was excluded from TPA. (Laypersons: She would have bled to death if she was given it due to the lung tumor)
I know this is the correct decision as devastating as it was to see the difference in results for her (partial paralysis without TPA versus being 99% fine with TPA). The ER folks were very wise in their choices and did take the time to explain everything.
Thank you very much for your postings!
We do CT angiography with a “quick and dirty” perfusion study right off the bat with our brain attack patients. That way we see the extent of the thrombus (vs ischemic migraine or Todds with unwitnessed seizure or dense residual TIA) and roughly how much brain is in play currently. I believe it lets us make more judicious choices with tpa and early endovascular intervention. We’ve had very few bleeds using this system.
The docs that advocate for the instant MRI are not the docs I would ever want for any of my family or for me. A good doc knows the system where they work. They know that a MRI of the brain takes a long damn time. In my facility you aren’t getting one period within the three hour window. You would have to show up three hours BEFORE you stroked to get your scan done on time. It’s because we are a Level 1 Trauma center, a major cancer center and we are by bed # the largest hospital in the city. Our six MRI’s run twenty four hours a day seven days a week constantly wildly overbooked with a two month non emergent waiting time.
Mostly because everyone keeps reading the media bs that MR is the very bestest diagnostic tool EVER and the family docs just cave.
The majority of our patient population is upper middle class and the filthy rich. No one has the nerve to bump one of these people out of the scanner even if all they are getting scanned is that troublesome cyst that just keeps coming back.
We live and die by CT. I know that CT is basically useless in showing subtle ischemia within the first twenty four hours but it is good at showing a bleed and that’s all we really care about before we go for the Tpa. We too are a “stroke certified” hospital with a two page checklist.
I have seen someone bleed to death after Tpa despite the fact they checked out. Tpa is a white knuckle drug every time you give it. I have seen Tpa work and fail. I have seen Tpa work but then the patient later bled at the infarct site and the catastrophic results were as if we hadn’t given it all.
I really hate any media reporting on any aspect of health care. They don’t understand, they make no effort to understand. All they want is to be able to write the basic Hollywood tearjerker with a happy ending.I guess because that is all anyone wants to read. It’s no different than watching ER and the miraculous recovery of the patient after twenty minutes of CPR, up walking, talking and ready for discharge without even a pimple.
Thanks to the media for making telling a family a patient has died so clearly impossible. Thanks for making the public assume because their family member died and House’s patient lived we obviously made some horrible error and we must now be sued.
How pissed off will I be if my next r/o CVA patients family member happened to have read that NY Times piece?
I’m a neurologist in the LA area. I practice at a well-regarded hospital (though its reputation exceed its grasp). Our hospital administration, and several of the neurologists on staff, are pushing vigorously to make our hospital a STROKE CENTER. The administrators don’t know diddly; its just the thing to do to look up to date, and they haven’t the faintest idea about the commitment required in terms of ER and neuroradiology support.
Here’s what happened two days ago:
I am called at 9:30 AM to see a 93 yo man who had had sudden-onset aphasia and R hemiplegia at 7:30 AM. CT was normal. I left my office (cancelling 2 nice patients) and went to the ER where I examined this fellow. I called the neuroradiologist, who confirmed that the CT was normal. I specifically asked if there was any evidence of hemorrhage or of hyperacute infarction, and he assured me there was none. I was strongly considering tPA (we were still w/in 3hr window) but on re-exam the patient was showing definite improvement. Also, the daughter, who had been given the standard spiel about tPA by a clinical pharmacist, was evidently told it was experimental, and was scared-off; I told her it was not experimental, but that there were certainly potential risks. In view of Pt’s improving condition I decided against tPA. That afternoon I got another CT (pacemaker, so no MRI) and there was a definite infarct in the Lt PCA distribution. And, reviewing the first CT gotten in the ER I could see the same infarct, though it had been read as normal! A 3rd CT next day confirmed that this was a new infarct, and not an old un-recognized one.
A couple of obvious issues:
First — the neuroradiologist (fully-trained) is an idiot. He specifically denied the lesion I had specifically asked about. I have had problems with him before; this was the worst.
Second — had I accepted his reading and had the patient not been improving I might well have given tPA. The risk of a major bleed with these early CT findings would have been quite high. A catastrophe for the patient and for all concerned.
Third — (excuse me for sounding a bit age-ist) — what if this had been a 40 or 50 year old man with a nasty, litigious family — same scenario — same major disabling or fatal bleed — same not a leg to stand on if a malpractice suit.
Fourth — this is a hospital that is gearing-up to be a STROKE CENTER. This was a staff neuroradiologist, not a general radiologist or a moonlighter.
Fifth — tPA is dangerous stuff. I can recall when IV tPA was given to patients w/ acute MI (without stroke symptoms or deficit — just MI) and occasionally they would inexplicably have cerebral bleed. Not sure why — maybe they did have an inapparant, asymptomatic cerebral embolus related somehow to their acute MI (?). Vividly remember a prominent USC professor whose career was cut short by this.
Sixth — Very odd that this current patient’s infarct would be visible on CT just 2 hrs after onset — it was not subtle, even though it was missed and CT mis-read. The history (from this man’s intelligent care-giver) was very definite and clearcut — OK to 7:30 and then an acute change. But the infarct looked more than 2 hrs old, and again that suggests increased risk.
I have had other serious problems w/ tPA in situation where it was used very appropriately, and I am very cautious w/ this drug. The data suggest it’s helpful, but I think it must be used very judiciously. IA tPA may be better if team can be geared up quickly enough. We’ve not used it yet.
Per Genentech Prescribing Information for Activase:
Indication: Activase is indicated for the management of acute ischemic stroke in adults for improving neurological recovery and reducing the incidence of disability. Treatment should only be initiated within 3 hours after the onset of stroke symptoms, and after exclusion of intracranial hemorrhage by a cranial computerized tomography (CT) scan or other diagnostic imaging method sensitive for the presence of hemorrhage (see CONTRAINDICATIONS in the full prescribing information).
The NINDS t-PA Stroke Trial, Part 2 3-Month Efficacy Outcomes and the NINDS t-PA Stroke Trial Safety Outcome studies:
Exploratory, multivariate analyses of both studies combined (n=624) to investigate potential predictors of ICH and treatment effect modifiers were performed. In Activase-treated patients presenting with severe neurological deficit (e.g., NIHSS > 22) or of advanced age (e.g., > 77 years of age), the trends toward increased risk for symptomatic ICH within the first 36 hours were more prominent. Similar trends were also seen for total ICH and for all-cause 90-day mortality in these patients. When risk was assessed by the combination of death and severe disability in these patients, there was no difference between placebo and Activase groups. Analyses for efficacy suggested a reduced but still favorable clinical outcome for Activase-treated patients with severe neurological deficit or advanced age at presentation.
————————————————————–
It is not experimental therapy. There have been multiple studies and many variables to consider and there will no doubt be changes in the above. Age would be a consideration. In any case there should be a hospital policy and procedure and protocol on the use of tPA in stroke for some protection in litigation and to prevent misuse.
Having been at a facility with an old single slice CT versus the new 64- or 256-slice CTs, would the CT unit itself have made a difference in the reading by the neuroradiologist? Some interventional radiologists are using tPA to dissolve blood clots in bladders. It’s a very expensive treatment versus bladder irrigation and it can potentially lead to a re-bleed. And yes, dissolving bladder blood clots with tPA is experimental / investigational therapy.
Excellent post. Thanks for speaking out about careful consideration! Kudos!
I am a 41 yo female – I had a stroke last September – I could barely speak or move my right arm/hand. I was luck to have IA tPA administered via an artery in my groin. Still seems Sci-Fi to me! :)
Except for a small bit of numbness in 2 fingers, I recovered fully with no PT or OT!
I credit the ER folks for making this phone call instead of pushing a full body throttle by the drugs. :)
I am a neuroogist in the Atanta area for about 20 yr. This whole thing is discusting
I can only give own single personal opinion, but I doubt most practicing neuroogists share the opinions of the ones quoted in the NYT article.l Do those guys realy see many patients or do they sit in ivory towers, revieing papers and teling others how smart they think they are?
I’m not competely convinced one way or the other if TPA is a goodthing(but it’s definately way overrated)
It seems these limited amount or people quoted are trying to pin us against each other ER docs, neuroogists etc. I don’t see this happen in real life in my neck of the woods
I have seen for years ER docs, FP docs. interists neuroogists and neurosurgeons take exceent care of people with strokes without the help of the government, JCHA, journalists/NYT and drug companies “unbiased data”
I know this is a dumb question but how much of this is financilly driven(by what looks like multiple recepients, but definately not true patients or those of us routinely taking care of them)
Whatever happenned to first do no harm?
I had a stroke Oct 4 and was given TPA within the 3 hr window. It was 2 blood clots and considered a major stroke. I was released Oct 7 from the hospital and feel good although a little weak on my left side and slight slurring of some speech. TPA saved my life.
BR Drexinger said
“I have seen for years ER docs, FP docs. interists neuroogists and neurosurgeons take exceent care of people with strokes without the help of the government, JCHA, journalists/NYT and drug companies “unbiased data”.
What is excellent care of stroke patients??? Heprin and a nursing home? There is “NO” other medical treatment for stroke patients at last I checked. What about the guidlines from the AHA/ASA? TPA has their highest recomendation when given within 3 hours and no contraindications are present. Do you just ignore the “unbiased data” reviewed by collegues to come to these guidline decisions?
If there were less of us that thought that “excellent care” has been given up to this point there would be no need for “the help of the government, JCHA, journalists/NYT and drug companies”.
Do you just ignore the “unbiased data” reviewed by collegues to come to these guidline decisions?
It’s the biased data that I ignore, which is a hell of a lot of it.
Then pay close attention to the National Institute on Health Data. That would be NINDS for the non medical folks. Cut and Dry 6.4 % SICH rate and a 1/3 more patients have minimal to no disability at 3 and 12 months. Distort the data however you choose but I’ve sat through many lectures from experts(in research and practice) in the field of stroke who live and practice by these data. Keep in mind that this was before imaging was any good, and SICH was defined as blood on CT and ANY change in NIH. NIH is very subjective and a 1 pt change could be seen very easily with no patient change at all by simply changing the person doing the rating. That’s why the definition of ICH has been changed for more recent studies such as SITS MOST (1.7% SICH)to 4 pt change and blood on CT. You can ignore drug company sponsored studies if you choose but 95% of all studies are funded by them. So if you blanket that philosophy you can’t posibly practice evidence based medicine. What do those of you that don’t use TPA do for your pts within 3 hours of stroke onset? Just curious? What are your outcomes? How do those compare to the current TPA data?
Why does it seem that every pro-tPA article (including NYT cited here) includes an anecdote about a patient who receives tPA and recovers immediately?
Has anyone actually read NINDS?
What is the short-term benefit from tPA for stroke? NONE!
IF you trust the data, the most you can claim is measurable benefit at 90-120 days.
The most recent trial (ECASS-3, telling us we can push the window to 4.5 hours) doesn’t even report data before 90 days.
So… to answer the question “What are your outcomes?”, most of us in the ED can only comment on our complications. Our successes will not been known (or knowable) for 90 days.
This is the mass media. Their job is entertainment, with at least a little basis in fact. “There is some quick cure for a major disease, but doctors haven’t gotten the message” is entertaining, in the sense that it grabs the attention (and thus readership for their ads). The degree to which it is true is of far lesser importance.
Diffusion MRI is SOC at the facility I’m associated with and are performed within 30 minutes of notification. All “code strokes” are run by neurologists 24/7. Seems like the ER docs like that as they can call any neurological symptoms a “code stroke” and dump the patient for a few hours. It also seems like an easy way for small town hospitals to transfer patients to the big city facility.
No offense to the ER docs, but it’s the neurologists that have to provide ongoing care to the patients in the hospital and at follow up, so they have a bit more skin in the game.
I’ve suffered several “mild” strokes, and the times that I arrived at the Emergency Room well within the three hour window, tPA was never offered as a viable treatment because my strokes were too “mild to treat”. Now I’m left with permanent brain damage and resultant cognitive losses and persistent left facial numbness and left calf muscle numbness. All because we have a bunch of ER doctors and neurologists in this country who more afraid of lawsuits and litigation and care less about preserving the brain and future of a stroke victim. I would have rather rolled the dice and faced death from a clot-busting medication than wind up the way I did from the strokes I suffered, and so would anyone else who’s suffered a stroke and is stuck with the residual effects and aftermath. ‘Nuff said.