Is tonight (Friday night). Our overnight shift, which on a Friday night can run from busy to very very busy.
The ‘switchover’ is at midnight, though for various technical reasons we won’t be fully electronic until after 3AM, so it’ll be a mixed environment of paper and electrons. I volunteered for this shift, so it’ll be a lot of fun.
I am cautiously optimistic, and we’ve given ourselves a big advantage: we’ve doubled up on scribes and we’ve “borrowed” them from places that already use the EMR (we’re on Epic, but it could be any system), and that should ease the transition. That, plus all the official tech helpers coming for the first 15 days.
We’re pretty well prepared for this, though it’s been described as starting a new job: I know the medicine but the ‘how’ and the ‘what are the cues we’re done’ are different. It’s billed as being mildly or very inefficient, though that’s supposed to get better with experience.
I’ll let you know.
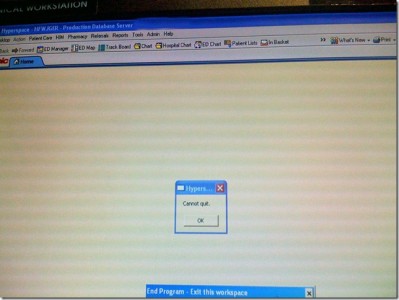
Update: The transition wasn’t smooth. There were much longer delays at each step that had been anticipated, the end result of which was the our 4AM doc was really the first doc to see the majority of their patients on the EMR.
It didn’t help that the ED was a total zoo. People will not stop having emergencies for us to smooth over our little technical problems. Imagine. (Yes, that was sarcastic, DWL).

Looking forward to the AAR, doc!
Good luck. I have been using EPIC for 3 years, and this past year our hospital added order entry. It certainly saved the hospital some money–they no longer have ward clerks! As for me, it adds a minimum of 10 to 20 minutes for each admission (I’m a hospitalist.) Good luck. I think EPIC is truly epic, and that there are alot easier systems.
BTW, the help desk is your best friend, it’s not their fault, they’re just doing their jobs…
You’ll do great and be loving the system shortly… after the growing pains wear off! Since you’re writing blog entries, you’re probably tech savvy and you’ll be off and flying in no time at all.
Your biggest frustration will probably your colleagues who aren’t as tech savvy. This is a big change for them and many will be kicking and screaming the entire way, maybe even sneaking paper when they can! Just encourage them to hang in there, offer tips when you can, and give pep talks to keep moral up.
Good luck!
My hospital adopted Cerner PowerChart about a year ago and although I have essentially mastered it I certainly don’t love it and agree with Marica it adds work for me, not reduces it. The PowerNotes module is awful and luckily I can still dictate my notes, but the poor ED docs aren’t allowed to dictate and as a result end up with lovely 5 page notes that tell you absolutely nothing.
EMRs do some things extremely well, mainly tracking down test results and notes from the past without wading through piles of charts. My big issue with them though is they do not replicate how most doctors think and aren’t very intuitive. Why do I have to scroll through a hundred choices to select an indication for prn Zofran? There’s only one reason I ever give it. The most common indication for EKGs at our hospital is abdominal pain since it’s at the top of the list and the ED docs don’t want to fart around finding the actual indication when they could be seeing patients.
There is automatic interaction-checking which sounds great until you’ve been reminded a thousand times of the same interactions you learned in medical school. I have learned the most dangerous substance at our hospital is the deadly Fleets enema, which seems to trigger an interaction with everything else on the formulary.
I could fill a page with my rants but suffice it to say EMRs are a decidedly mixed blessing.
How’d it go, Doc? I hope well. Since I do data modeling and programming, I’m very interested.
EMR has turned us into secretaries. We spend an unbelievable amount of time documenting, entering orders, medication reconcilliation, work excuses. It has hurt our productivity. Admin loves it as the hospital billing has skyrocketed. Please let me know how you work out the scribe issue. Will you need 2 scribes per MD? I don’t see it working well with one.
You will find the charts very generic and God help you if you have to rely on it 2 years from now in court. The consultants hate our charts as they can not easily find the substance of the chart due to 20 entries that the bed rails are up and monitors attached.
On a positive note they do help keep track of labs.
Gunner, the hospital adminbots love something?!?!!? Oh wait it involves money….thats why!
Here in the great socialistic state of madison, wi; my oncology clinic just went EPIC!!!! Did you hear the TA-DAH!!! No, hm…
Well actually the epic drones were in the office for 5 weeks trying to train us on the intricacies of epic. They pushed, they prodded, they cajoled…and we finally caved in.
Actually, it was very amusing to watch the human drama unfold. What with THEM not knowing SQUA-DUSH about OUR work flow. And THEIR insistance that we must follow or be eliminated….no not really…just felt that way.
Sigh, I think the telling point was when one of the trainers stated, “It’s not our responsibility to figure out your work flow…its our responsibility to tell you which buttons to push.”
Oh Lord a Goshen you just pushed a couple there missy!!!!!!
Steve
cerner has turned my life as a nurse into a living hell….when you’ve made 4 phone calls to the help desk (somewhere outside of the u.s.) to resolve freezing screens and computers that can’t find wherethey are and a host of other problems, you know you’re in trouble when the help desk guy tells you to wait a minute he has to reboot his screen…sigh. 5 minutes with the patient and 20 minutes to chart it..talk about an inverse ratio