This article and its graph (from the NEJM), and its interesting, informative but probably useless graph, was referenced today on twitter, via the Washington Post’s Wonkblog,
Recently, the Centers for Medicaid and Medicare Services announced a scheduled cut in Medicare physician fees of 27.4% for 2012. This cut stems from the sustainable growth rate (SGR) formula used by the physician-payment system. …
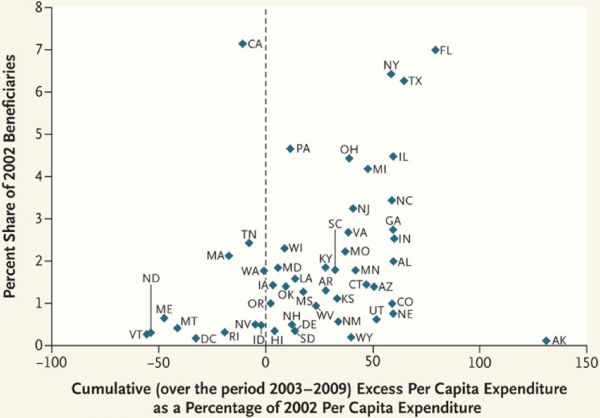
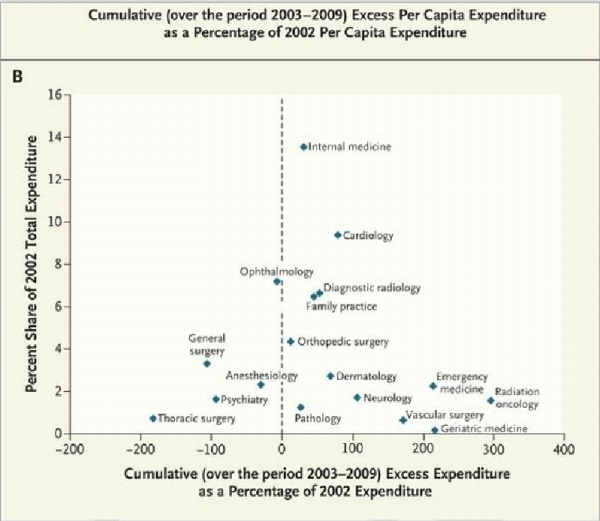
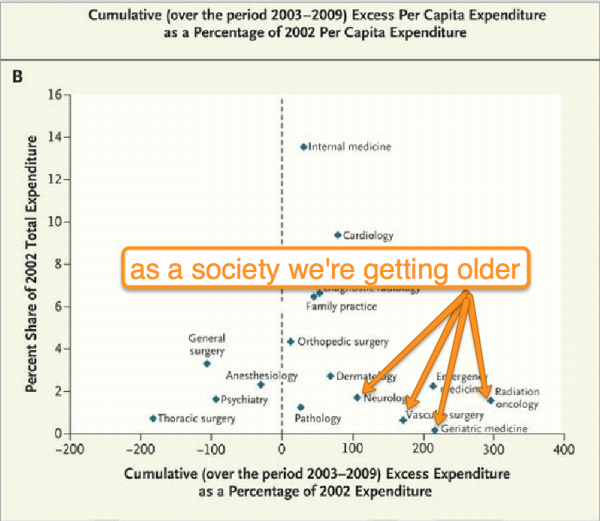
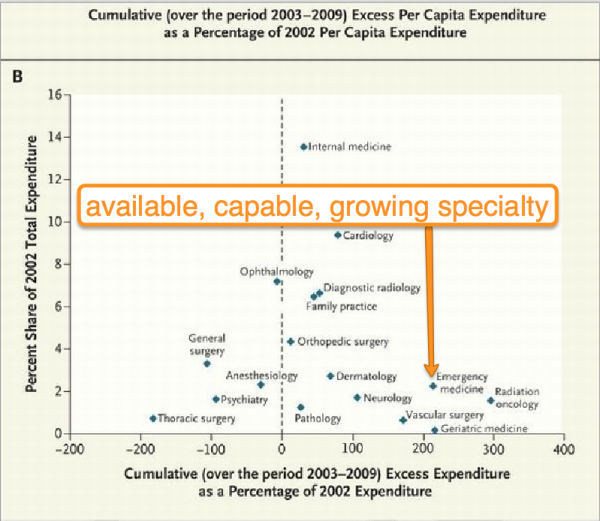
To illustrate the level of inequity in this system, we broke down the national spending for Medicare physician services by state and by specialty and determined which states and specialties have contributed most to the SGR deficit between 2002, when the program was last balanced, and 2009. Although SGR spending targets are set on a national level, we computed state targets by applying the SGR’s national target growth rate to each state’s per capita expenditure, using 2002 as the base year. Our analysis is an approximation, because, unlike the SGR, we do not adjust for differential fee changes. …We compared the state targets for the years 2003 to 2009 to actual state expenditures and added the annual difference between these figures to get a cumulative difference between the state’s spending and the SGR target. This cumulative difference was then divided by the 2002 per capita expenditure to determine the percentage growth since 2002.
Here are the graphs, and my attempts at explanation, and the questions I have:
Hmm. First, was a rebalancing done on the numbers of citizens in these states between 2002 and 2009? Texas was a net in-migration state during this time period, NY was a net out, and Florida was a mixed bag (source: Brookings .pdf). Hmm. (And, Alaska was mid-pack throughout). I’ve never understood regional variations in billing.
The By Specialty graph:
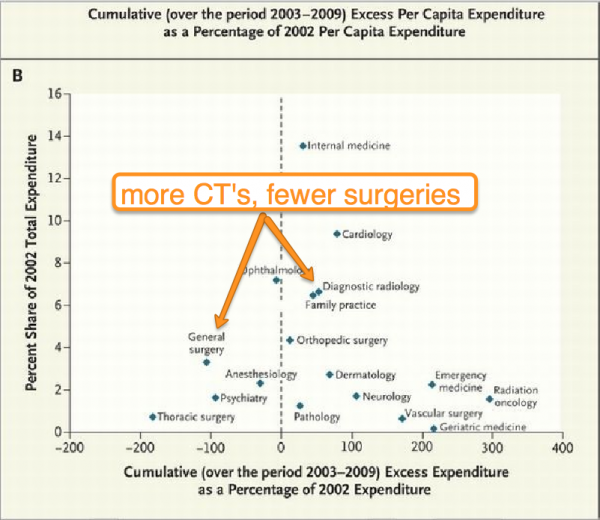
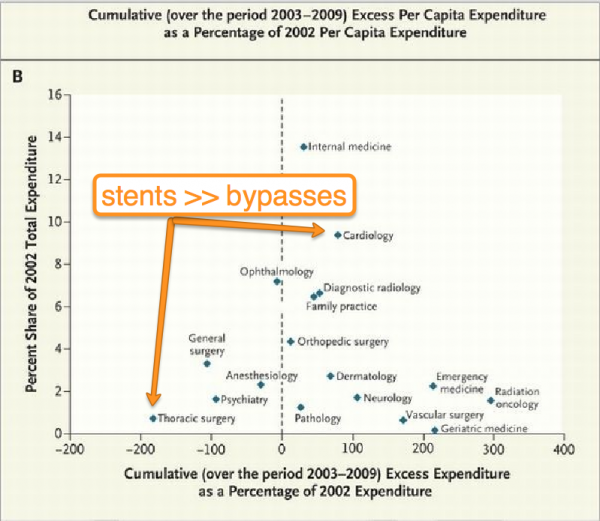
And, my half-joking explanations, in the slides:
Yeah, okay, that’s EM gloss. Our costs went up, and our volume went up, and now everyone either wants or gets a CT scan. That’s not a huge surprise.
Interesting, nonetheless.